|
The difference between chronic pain and chronic pain syndrome is sometimes difficult for people to understand. Chronic pain is simply pain that has continued for a long time. If pain has persisted for six months or longer, it is generally regarded as persistent or chronic, unless there is some clear reason as to why the pain has continued. The term chronic pain syndrome has fallen into disuse by many people due to the idea that it may lead professionals to think that the cause of the continued pain has been clearly identified, when the problem of chronic pain is very complex and far from solved. The term chronic pain syndrome is likely to persist over time, as it was recognized as a disability in legal terms and therefore is still regarded by some as a useful concept from the legal point of view. Further, the term chronic pain syndrome was dropped in favour of making specific medical and psychiatric diagnoses, yet the psychiatirc diagnoses "Pain Disorder Associated With Psychological Factors" and "Pain Disorder Associated With Both Psychological Factors and A General Medical Condition" has criteria that are less precise than the old diagnosis of chronic pain syndrome. Many psychologists have started using the newer diagnostic labels, but still use the old criteria for chronic pain syndrome as general guidelines.
The diagnoses are generally made when a person's pain becomes the central problem, rather than the medical condition that precipitated the pain. This can occur when dagnostic testing has failed to reveal any clear medical problem, but often occurs when there is a clear medical condition that is presumably causing the pain, but there is no further medical treatment that is likely to benefit the person. In this writer's experience the Pain Disorder diagnoses are most appropriately made on the basis that the methods used by medical professionals and the person with the persistent pain are clearly not benefitting the persn and may be causing the person more harm than good. This is somewhat different from the situation in which medical diagnoses have been made, but the medical practitioners have stated that the person is reporting more pain for longer than expected. Statements like this are still made by many medical practitioners, but clearly there is little or no data to help one can judge how much is too much or how long is too long. In Psychology such judgments are usually based on the mean and standard deviation of some measure or combination of measures, and this kind of statistical data is lacking for various medical conditions. Thus, the specific duration and intensity at which pain becomes chronic is not known.
How does one know whether the diagnoses might be appropriately considered? In many instances, there is no reason to consider these diagnoses. The duration of pain beyond some unknown point in time is not a very good reason to conclude that psychological factors are playing a role in the maintenance of pain. There are rare instance wherein psychological factors can lead directly to physical disorder. Extreme psychological stress can cause medical conditions such as seizures or psychogenic blindness, but these cases are very rare and usually there is no question that the psychological factors are primary. These cases do not often involve any type of physical injury and clearly involve psychological injury, whereas many of the cases referred for evaluation of Pain Disorder have clear physical injury and persisting pathology.
However, it is sometimes the case that the person's behaviour and strategies for coping with pain are dysfunctional. If, for example, the person avoids getting out of a wheelchair for fear of pain and medical opinion is that the wheelchair is detrimental to the person's physical health, then a diagnosis of Pain Disorder might serve to alert caregivers that this is a problem. Many people continue to take opioid medication far beyond the recommended length of time. While this does not usually take the form of an addiction, tolerance to the medication does develop and this can be a preoblem in itself. Tolerance is one determinant of "rebound pain", which means that the person has more pain than they would ordinarily have as the medication wears off, because the person's body is used to a certain level of medication. If there is some degree of rebound pain, the person will not be able to manage this pain in any other way except through medication as it is the lack of regular dosing of medication that is the problem. Continuing to take the medication is a temporary solution, whereas managing the pain through regular paced activity might be a better long-term solution, especially because opioid medications have side effects including drowsiness and depression, and the side effects tend to escalate as the dosage increases. In a sample of patients assessed at a chronic pain treatment facility (the PACE program, formerly known as the BEEP program) in British Columbia, the amount of medication was positively correlated with ratings of pain, depression (measured by Beck Depression Inventory), and disability (measured by Pain Disability Index). This is the oposite of what would be expected if medication was helpful to these clients.
If a Pain Disorder is suspected, the person might benefit from a multidisciplinary or interdisciplinary assessment. These assessments are often conducted by teams of professionals skilled in managing chronic pain problems. The teams may include physicians, psychologists, physiotherapists, occupational therapists, nurses, and massage therapists. These teams can help the person to deal with the various facets of their condition. The physician can educate the person on their medical condition and ensure that all medical treatments and investigations have been tried. The psychologist can assist the person in seeing and trying new ways of managing pain, and help them overcome barriers to changing their habits and behaviors. Physiotherapists can recommend exercises designed for long term management rather than short term gains. Occupational therapists can assist them in managing tasks at home and in the workplace so that they can resume many of their former activities without causing more pain.
Although many of these patients seem beyond the ability of the medical system to help, interdisciplinary programs can assist a large proportion of these individuals return to most of their activities, while managing pain more effectively. 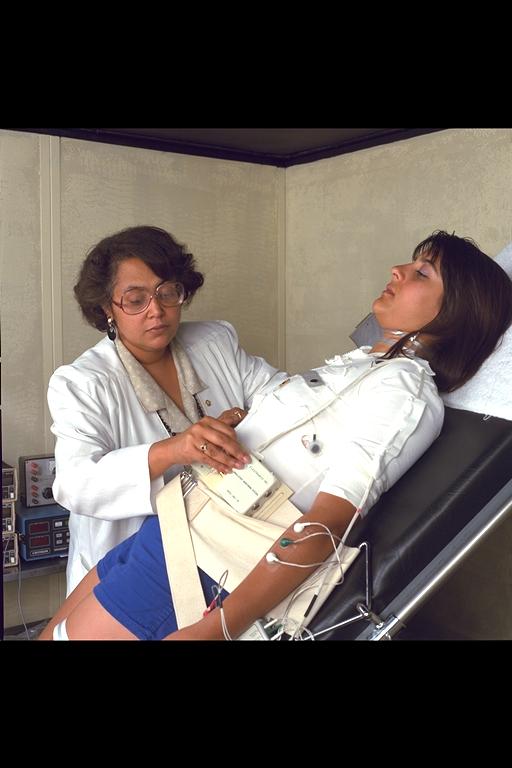
|

